Cataracts surgery is a common procedure aimed at improving vision for individuals suffering from cataracts. Cataracts refer to the clouding of the lens in the eye, leading to blurry and hazy vision. This article will delve into the various aspects of cataracts surgery, including what cataracts are, the surgery process, the benefits it offers, as well as the potential risks and complications involved. By the end of this article, you will have a better understanding of cataracts surgery and be able to make an informed decision about whether it is the right choice for you.
cataracts surgery is a procedure that offers numerous benefits for individuals experiencing vision problems due to cataracts. By understanding what cataracts are, the surgery process, the benefits it provides, and the potential risks involved, you can make an informed decision about whether cataracts surgery is the right step for clearer vision and an improved quality of life.
What are Cataracts?
Cataracts are a common eye condition that primarily affects older adults but can occur in anyone, including newborns. The science behind cataracts involves the gradual degradation of the protein in the lens of the eye, leading to its cloudiness. As a result, light cannot pass through the lens properly, causing vision problems.
Common symptoms of cataracts include blurry vision, difficulty seeing at night, sensitivity to light, and seeing halos around lights. As cataracts progress, activities like reading, driving, and recognizing faces become increasingly challenging.
It is interesting to note that cataracts can develop in one or both eyes and may progress at different rates. Factors such as age, genetics, certain medical conditions like diabetes, prolonged exposure to sunlight, smoking, and eye injuries can increase the risk of developing cataracts. Additionally, some studies suggest that a diet rich in antioxidants and certain vitamins may help prevent or slow down the progression of cataracts.
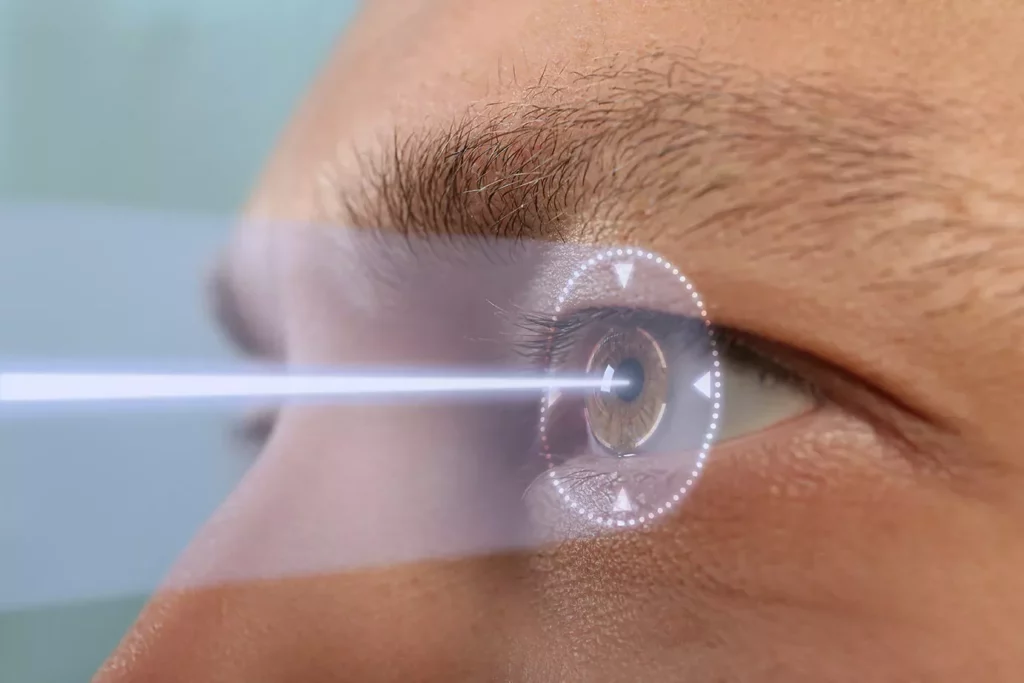
When cataracts start to interfere significantly with daily activities and quality of life, surgery to remove the cloudy lens and replace it with an artificial one is a common and highly successful treatment option. Cataract surgery is one of the most commonly performed procedures worldwide, with a high rate of success in improving vision and overall quality of life for patients. It is typically a quick and relatively painless outpatient procedure that has evolved significantly over the years, with advancements such as laser-assisted cataract surgery offering even more precision and better outcomes.
The Process of Cataracts Surgery
Pre-Surgery Preparations
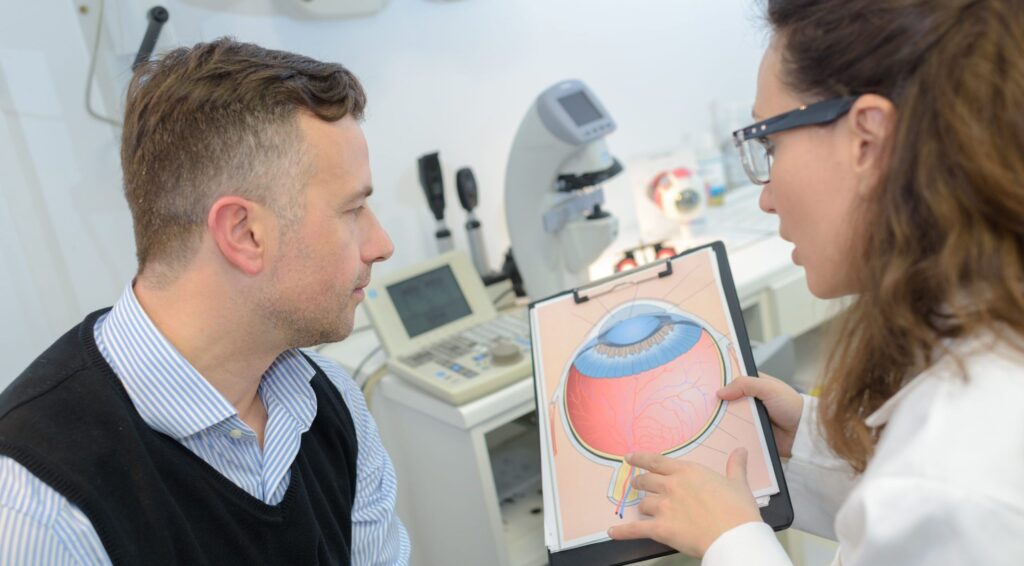
Before undergoing cataracts surgery, several preparatory steps need to be taken. This usually involves a comprehensive eye examination to determine the severity of the cataracts, the overall health of the eye, and to ascertain the most suitable type of surgery. Your eye doctor will carefully assess your visual acuity, evaluate the extent of the cataracts, and discuss the potential benefits and risks of the procedure with you.
In addition to the eye examination, your doctor will also review any medications you are currently taking and provide instructions for their use before and after the surgery. Certain medications may need to be temporarily discontinued or adjusted to ensure optimal surgical outcomes. It is crucial to communicate any allergies or sensitivities you may have to medications, as this information will guide the medical team in selecting the most appropriate anesthesia and post-operative medications for you.
Furthermore, it is important to arrange for transportation to and from the surgical facility, as well as a companion to assist you during the initial recovery period. This ensures your safety and comfort, as you may experience some temporary vision changes and drowsiness immediately after the surgery.
The Surgery Procedure
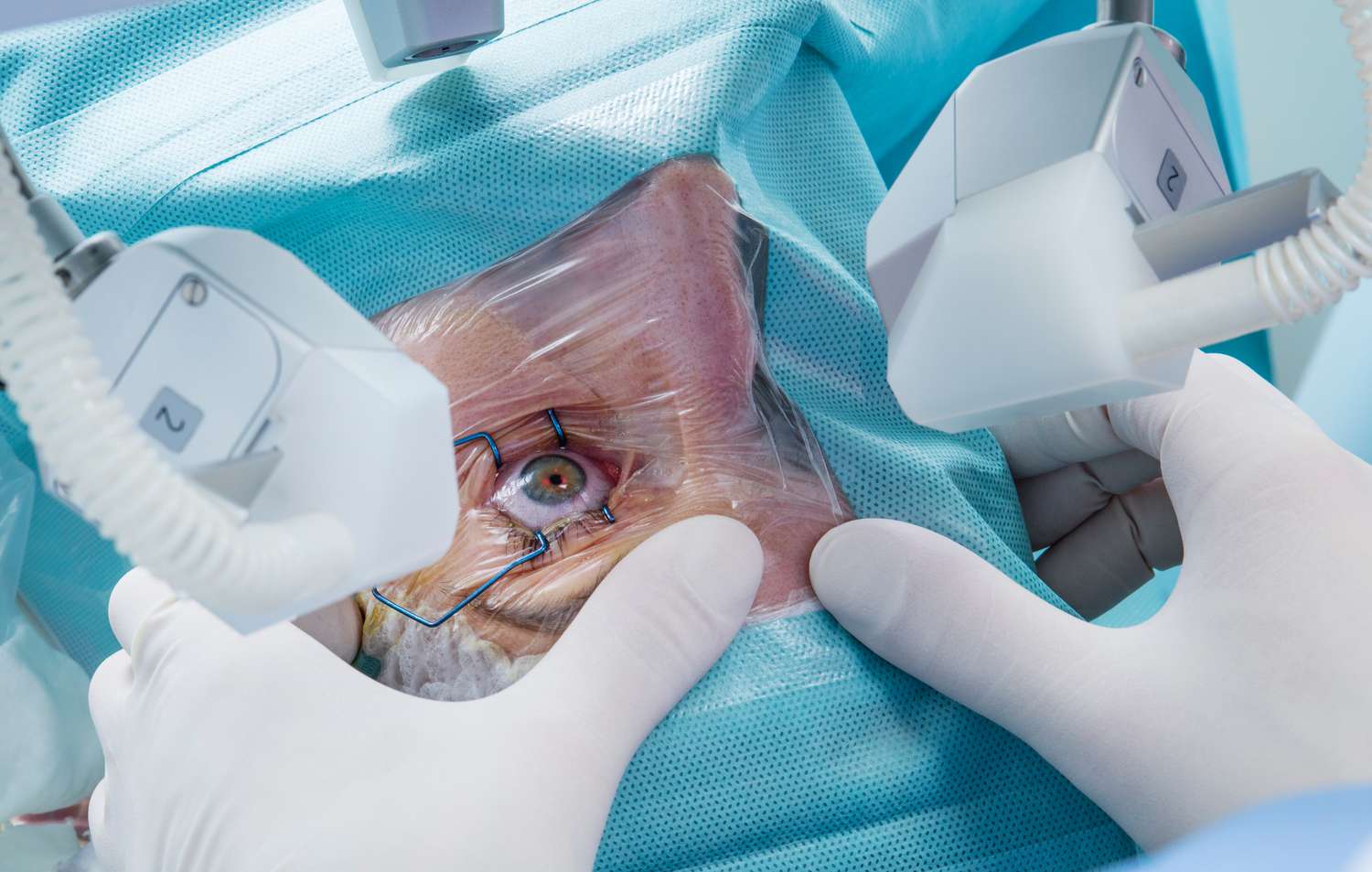
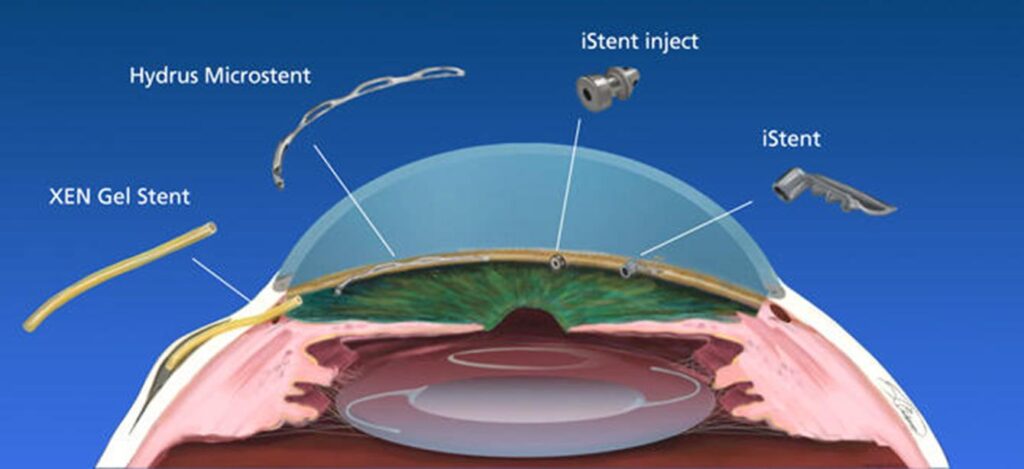
Cataracts surgery is typically an outpatient procedure, meaning you can return home the same day. The surgery itself involves the removal of the cloudy lens and its replacement with an artificial intraocular lens (IOL). There are different types of cataract surgery, including phacoemulsification and extracapsular extraction, which your doctor will discuss with you based on your individual case.
During the surgery, you will be positioned comfortably on an operating table, and the surgical team will ensure your relaxation and well-being throughout the procedure. The surgeon will make a small incision in the eye, break up the cataract using ultrasound waves, and remove it. The IOL, carefully selected to match your specific visual needs, is then inserted into the lens capsule, positioning it to focus light correctly onto the retina. Read more about relaxation at https://www.health.harvard.edu/mind-and-mood/six-relaxation-techniques-to-reduce-stress
The entire procedure usually takes less than an hour, and patients are either given local anesthesia or sedation to ensure comfort throughout. The use of advanced surgical techniques and equipment, coupled with the expertise of the surgical team, minimizes the risk of complications and maximizes the chances of a successful outcome.
Post-Surgery Care and Recovery
Following the surgery, you will be given specific instructions on how to take care of your eye during the recovery period. This typically includes using prescribed eye drops to prevent infection and reduce inflammation. It is important to follow the recommended dosing schedule and maintain proper hygiene to ensure optimal healing.
During the initial stages of recovery, it is essential to protect your eye from irritants and avoid activities that could strain your eyes, such as heavy lifting or bending over. Your doctor will provide guidance on when it is safe to resume normal activities, including driving and exercising.
Your doctor will schedule follow-up appointments to monitor your progress and to ensure proper healing. These appointments are crucial for assessing your visual acuity, checking the stability of the IOL, and addressing any concerns or questions you may have. Most patients experience improved vision within a few days, with complete recovery achieved after a few weeks. During this time, it is common to have mild discomfort, sensitivity to light, and blurred vision, but these symptoms gradually subside as your eye heals and adjusts to the new lens.
The Benefits of Cataracts Surgery
Immediate Improvements in Vision
One of the key benefits of cataracts surgery is the immediate improvement in vision. Patients often report clearer and sharper vision post-surgery, allowing them to engage in daily activities without the hindrance of blurred vision. Colors appear more vibrant, and visual acuity is significantly enhanced, leading to an improved overall quality of life.
After cataracts surgery, many patients experience a newfound sense of freedom and independence. Tasks that were once challenging due to poor vision, such as driving at night or reading small print, become much easier. The joy of being able to see clearly again after struggling with cataracts for so long is immeasurable.
Long-Term Health Advantages
Aside from the immediate benefits, cataracts surgery also offers long-term health advantages. By removing the cloudy lens and replacing it with an artificial one, the risk of developing other eye conditions, such as glaucoma or age-related macular degeneration, is reduced. Furthermore, studies have shown that cataracts surgery may also contribute to a decreased risk of falls and fractures in elderly patients.
Moreover, improved vision from cataracts surgery can have a positive impact on mental health and overall well-being. Being able to see clearly can boost confidence, increase social interactions, and prevent feelings of isolation that can sometimes accompany vision loss. The ability to fully engage with the world visually can lead to a more active and fulfilling lifestyle.
Potential Risks and Complications
Understanding the Risks
Like any surgical procedure, cataracts surgery carries certain risks. While the overall success rate is high, there is a small chance of complications. This can include infection, bleeding, inflammation, and changes in eye pressure. Your eye doctor will thoroughly explain these risks to you and answer any questions you may have, ensuring you have all the necessary information before making a decision.
It’s important to note that while these risks exist, cataract surgery is one of the most commonly performed and safest surgical procedures in the world. The vast majority of patients experience significant improvement in their vision and quality of life after undergoing the surgery. With advancements in technology and surgical techniques, the likelihood of experiencing complications has significantly decreased over the years. To learn more about advancements in technology click here.

How to Mitigate Potential Complications
To mitigate potential complications, it is crucial to follow all post-surgery instructions provided by your doctor. This includes taking prescribed medications, attending follow-up appointments, and avoiding activities that may strain your eyes. It is also advisable to promptly contact your doctor if you experience any unexpected symptoms or concerns during the recovery period.
Furthermore, maintaining good overall eye health through a balanced diet rich in nutrients like vitamin C and E, wearing sunglasses to protect your eyes from harmful UV rays, and avoiding smoking can also contribute to a smoother recovery process and reduce the risk of complications. By being proactive in your eye care and following your doctor’s recommendations diligently, you can increase the likelihood of a successful cataract surgery outcome and enjoy clear vision for years to come.
Making the Decision: Is Cataracts Surgery Right for You?
Factors to Consider
When considering cataracts surgery, it is important to take various factors into account. These can include the severity of your cataracts, the impact they have on your daily life, and your overall health. Additionally, discussing your concerns and expectations with your eye doctor can help you make an informed decision and determine if cataracts surgery is the right course of action.
Furthermore, it is essential to consider your lifestyle and activities that may be affected by cataracts. For instance, if you enjoy driving or reading, impaired vision due to cataracts can significantly impact your ability to engage in these activities. Understanding how cataracts are limiting your daily life can provide valuable insight into the necessity of surgery.
Talking to Your Doctor about Cataracts Surgery
If you are considering cataracts surgery, it is advisable to consult with your eye doctor. They can provide a thorough evaluation, discuss the potential benefits and risks of the procedure, and address any concerns you may have. This open dialogue will allow you to make an educated decision and proceed with confidence if cataracts surgery is recommended.
Moreover, discussing the financial aspect of cataracts surgery with your healthcare provider is crucial. Understanding the costs involved, including pre-operative assessments, the surgery itself, and post-operative care, can help you plan accordingly and alleviate any financial stress associated with the procedure. Your doctor can also provide information on insurance coverage or financial assistance options available for cataracts surgery.
Read more